Pain is the vital indicator that pirates a shift. It complicates triage, clouds assessment, and, when dealt with poorly, deteriorates client trust fund. Yet couple of medical professionals obtain thorough training suffering scientific research and functional analgesia beyond the essentials of ladder-based prescribing. The ideal brief course can close that gap without thwarting your routine, using focused frameworks you can take back to clinic tomorrow. The very best alternatives mix pharmacology and procedural abilities with interaction, risk mitigation, and documentation, after that award a pain monitoring certification that lugs weight with employers and regulators.
This overview makes use of years of functioning along with emergency medical professionals, pain doctors, nurses, and allied health and wellness medical professionals that deal with discomfort at every stage, from the first IV morphine press to long-game rehab. It will assist you choose a pain administration training course that fits your scope and your fact, whether you function evenings in ED, run a busy basic practice, or help people relocate once more as a physiotherapist.
Why medical professionals look for brief training courses now
Two points can be true at once. Analgesia saves lives and protects function, and analgesia can damage if we overreach or ignore threat. Over the last years, recommending has actually tightened, laws have actually stiffened, and people have much more complicated multimorbidity. That growing stress appears in the ward when an individual with chronic neck and back pain needs secure postoperative control, or in the area when someone who attempted an on the internet health and fitness challenge offers with tendinopathy and a background of depression.
Short programs suffering management fulfill medical professionals where they are. A good program updates your mental versions, not just your medication dosages. It clarifies when to use ketamine as opposed to intensifying opioids, just how to guidance on expectations, and just how to record choices that could be evaluated later on. For nurses and physiotherapists, targeted pain management training broadens range within risk-free boundaries and highlights where collaboration makes treatment better.
The composition of a high‑value pain administration course
The best pain administration programs, whether marketed as a discomfort management qualification course or a certification training course suffering monitoring, share a couple of attributes. They straighten with clinical truth, they incorporate proof with lived experience, and they make time count.
Expect the adhering to columns:
- Pragmatic pharmacology. Not simply systems, yet side-by-side comparisons of oral, IV, and local alternatives with context. As an example, when to make use of oral NSAIDs for kidney colic versus IV ketorolac, or how to dosage intranasal fentanyl in a child with a forearm crack when IV access can wait. Multimodal strategy. Genuine instances that combine acetaminophen, NSAIDs, local methods, and, if needed, low-dose ketamine or opioids. Programs that design these bundles aid you relocate past single-agent thinking. Communication and expectation setup. Short manuscripts and role-play for acute and chronic contexts. You discover exactly how to explain useful goals and timeframes, set borders around opioids, and straighten plans with a client's story. Documentation and danger oversight. Clear guidance on risk tools, pee medicine screening when appropriate, PDMP checks where they exist, and therapy agreements, without turning the check out into a list exercise. Procedural exposure. For ED and immediate treatment, emergency situation pain monitoring frequently includes ultrasound-guided nerve blocks, hematoma blocks, and breathed in analgesia. Even a half-day lab makes a measurable distinction on your following shift.
When a program declares to provide pain monitoring certification, search for transparent learning objectives, called professors with medical practice, evaluation beyond presence, and a certificate that states proficiencies, not simply hours.
Matching program kinds to scope and setting
Pain looks various in each clinic, therefore need to training.
Acute care and ED. Emergency medical professionals need speed, procedures, and step-by-step skills. A brief emergency situation discomfort administration course that trains you to do a fascia iliaca block, take care of extreme migraine with non-opioid pathways, and use low-dose ketamine safely will repay itself within a couple of shifts. Simulation that includes managing hypotension after IV opioids or frustration with ketamine is invaluable.
Primary care and healthcare facility medicine. Right here the difficulty is continuity. You need a structure for severe on chronic pain, post-op pain in patients already on lasting opioids, and tapering conversations. A certification course hurting administration that includes deprescribing approaches, non-pharmacologic techniques, and shared decision making will certainly tighten your practice.
Nursing. Discomfort monitoring training for registered nurses should highlight evaluation ranges across populaces, titration methods, PCA safety, and non-pharmacologic techniques like assisted breathing or chilly and warm therapy. Discomfort administration training courses for registered nurses that include scenario-based knowing on delirium risk, respiratory surveillance, and paperwork decrease unfavorable occasions and boost client satisfaction.
Physiotherapy and allied health and wellness. Pain administration courses for physio therapists are most handy when they translate pain neuroscience into clinical language patients understand. Anticipate components on graded exposure, pacing strategies, flare-up management, and just how to collaborate with prescribers. If the program consists of short motivational speaking with method, you will utilize it every day.
Advanced students and GPs with unique rate of interest. A pain management accreditation training course that includes basic interventional ideas, opiate stewardship, and paths for neuropathic discomfort will position you as a regional source. Great programs likewise reveal when to refer and how to coordinate with dependency services.
A closer check out PUAEme008 and instant care
Many clinicians experience the code PUAEME008 in course summaries. In a number of territories, this system concentrates on supplying pain administration in prehospital or initial action contexts. If your practice consists of out-of-hospital treatment, remote facilities, occasion medication, or commercial sites, a puaeme008 offer discomfort management unit can be the core you need.
The puaeme008 unit typically covers:
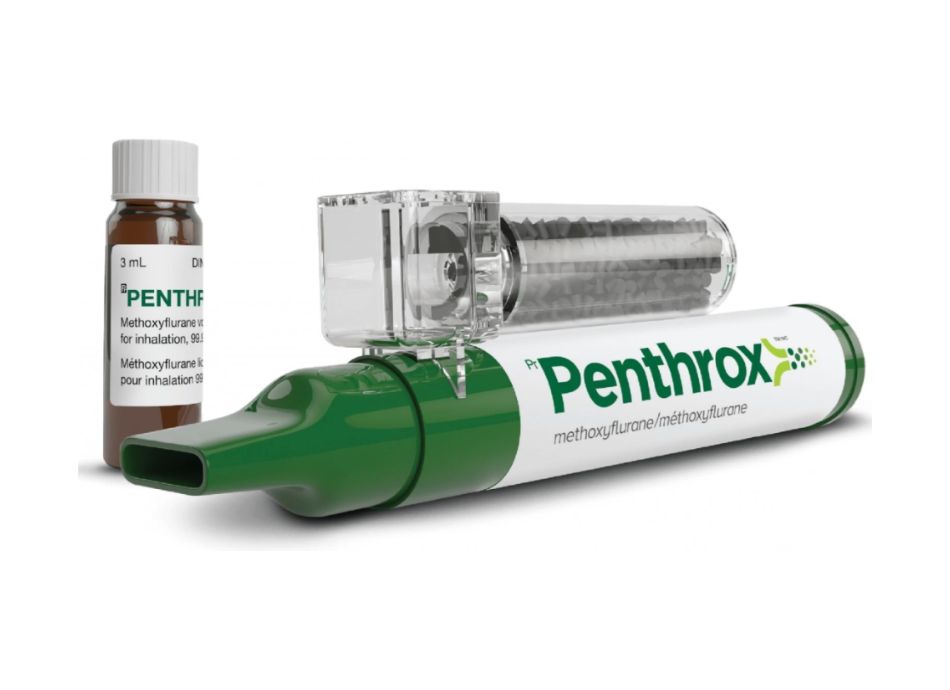
- Rapid pain analysis, consisting of spoken and functional ranges throughout ages. Safe use inhaled analgesia like methoxyflurane, intranasal fentanyl, and IM or IV choices within scope. Contraindications and red flags for time-critical transfer, such as area syndrome danger, abdominal catastrophes, or developing neurologic deficit. Documentation needed for handover and legal protection. Scene and group safety and security, including dealing with onlookers and taking care of restricted resources.
If you prepare to offer pain management skills training discomfort management program content for very first responders or paramedics, examine that your distribution maps to puaeme008 demands, consists of monitored abilities verification, and details medications within the -responders' lawful extent. Programs that align with puaeme008 offer pain monitoring are particularly beneficial to facility-based clinicians who periodically work in austere environments.
What "qualification" actually means
The language around discomfort administration certificate and pain administration certification can be slippery. Some programs offer a certificate of completion for proceeding education and learning hours. Others confer an official credential acknowledged by an university or board. Both can help, however they offer various purposes.
Ask 3 questions:
- Who identifies the certificate? If it is backed by a professional college, a nursing board, or a healthcare system, it is more probable to affect credentialing or privileges. What proficiencies are evaluated? Participation is not skills. Search for skills checklists, case-based examinations, or OSCE-style assessments. How long is the recognition valid? A certificate that expires after two years pushes you to rejuvenate as guidelines change.
Short courses in pain administration that culminate in reliable qualification signal to your team that you have bought a skill set beyond standard training. For nurses, this can support increased duties with PCAs or procedural sedation tracking. For physiotherapists, it may support innovative duties in relentless pain programs. For medical professionals, it may help when working out methods or chairing a discomfort stewardship committee.
What you can discover in a weekend that still matters a year later
A two-day pain monitoring training can hardwire routines if the web content is anchored to scientific moments you identify. Consider a few instances from practice.
Migraine in the ED. A training course that shows a procedure making use of IV fluids, metoclopramide, magnesium, and ketorolac minimizes opioid direct exposure and enhances throughput. You learn to expect akathisia and treat it preemptively with diphenhydramine. You get scripting for discharge that covers triggers, step-up strategies, and when to return.
Hip crack in the elderly. Ultrasound-guided fascia iliaca blocks can reduce opioid dosages by fifty percent or more. In a skills lab, you exercise probe handling, identify the femoral artery, and view anesthetic spread. Next change, a client with a neck-of-femur fracture comes to be settled within 20 mins, with less episodes of ecstasy overnight.
Neuropathic pain in health care. As opposed to layering weak opioids over gabapentinoids, you find out a path that starts with education and learning, rest hygiene, and duloxetine or low-dose TCAs with clear surveillance. You prepare a two-step follow-up and established a functional statistics, such as 15 minutes longer on the stationary bicycle within six weeks.
Acute low pain in the back with red flags missing. You exercise a five-minute explanation of discomfort physiology, guaranteeing language regarding the natural training course, a brief prescription for NSAIDs if endured, and a return-to-activity strategy. You stay clear of unnecessary imaging and furnish the client with indication for re-evaluation.
These gains accumulate. After a reliable pain management training course, your prescribing profile changes, your documentation tightens up, and your patients really feel even more heard.
Choosing among formats without shedding a week of clinic
Time is the restriction. Programs that balance online sessions with self-paced components produce the very best retention for busy clinicians.
Live workshops. Hands-on elements matter for nerve blocks, breathed in analgesia setup, and PCA tool programming. If you require step-by-step self-confidence, prioritize at least one complete day of in-person abilities practice with faculty feedback.
Synchronous virtual sessions. Helpful for case conversations, role-play, and debriefing tricky situations. Breakout spaces that imitate consults or tough conversations are remarkably effective.

Asynchronous modules. Pharmacology updates, guideline recaps, and documents requirements translate well to video and reading. Look for a system that tracks development and allows fast reference later.

Hybrid models commonly provide you the practical benefits without travel. For instance, an emergency situation discomfort monitoring workshop may provide pre-course video clips on ketamine physiology, then concentrate online time on sedation lists and nerve block technique.
Pitfalls to avoid when scanning brochures
Marketing language can obscure the actual worth. Focus on signals of deepness and integrity.
Faculty with active scientific roles. A pharmacologist that still takes call or a registered nurse teacher with current ward experience will certainly anticipate your discomfort points.
Case granularity. Unclear situations seldom transform practice. Look for programs that force you to make decisions with insufficient data, defend your plan, and reflect on outcomes.
Scope clearness. Pain monitoring courses for registered nurses should not imply independent suggesting if your territory does not allow it. Discomfort administration training courses for physio therapists should not oversell medical management. Clear interprofessional boundaries make cooperation smoother.
Assessment that values your time. A 25-question multiple-choice test can examine recall, yet a short structured instance article examinations application. Like the latter.
Follow-up resources. After the program, you require quick-reference dosing tables, client education leaflets, and lists. If you can not discover them at 3 a.m., they will certainly not help.
Documentation that safeguards clients and clinicians
Courses worth your money show paperwork that shows medical reasoning, not simply boxes ticked.
Key components to capture:
- Pain tale and useful influence, consisting of rest and mood. For chronic discomfort, listing what the person can do today and what they want to regain. Risk review. Prior overdose, substance use, sleep apnea, renal or hepatic disease, allergic reactions, QT-prolonging meds. Rationale for chosen methods. Explain why you integrated acetaminophen and NSAIDs, why you included low-dose ketamine, or why you avoided opioids. Safety plan. Bowel programs if opioids are used, sedation warnings, driving warns, and clear return parameters. Follow-up and contingencies. That will evaluate the plan and when. If tapering, compose the schedule in milligrams and in simple language.
When auditors or colleagues read a graph such as this, they comprehend your selections. People understand them too.
The actual benefit of multimodal care
The term multimodal obtains sprayed till it loses meaning. In technique, it resembles this: a client with a distal span crack receives a hematoma block, then dental acetaminophen and advil, a sling, and support for elevation and topping. They leave without opioids, discomfort is tolerable, and sleep is feasible. Or a client with persistent post-surgical discomfort obtains a mixed plan of rated task, duloxetine, and a short training course of topical NSAIDs, with clear objectives. Results improve not since one medicine is wonderful, but because the strategy appreciates physiology and habits both.
A strong discomfort monitoring training program will make multimodal treatment force of habit. You stop reaching reflexively for dosage accelerations and begin sequencing modalities with intent.
For instructors wanting to offer discomfort monitoring course offerings
If you intend to give pain administration training programs within a medical facility, a regional network, or a specialist body, a couple of style choices figure out whether your program sticks.
Start with regional data. Draw a month of certificate course in pain management suggesting records or ED length-of-stay metrics for pain presentations. Utilize them to pick components that deal with genuine gaps. If opioid administration peaks at 4 a.m., think about an overnight simulation or microlearning push.
Build interprofessional groups. Combine an ED physician with an elderly nurse and a physiotherapist for co-taught sessions. Each brings various lenses. The nurse translates surveillance and side effects right into bedside activity, the physiotherapist maps activity strategies, and the doctor structures risk and pharmacology.
Map to acknowledged systems. Where pertinent, align content with systems like puaeme008 provide pain monitoring. If your students require pain management qualification aligned to a board or college, safe and secure recommendation very early and layout analyses to match.
Design for reinforcement. Deal a short follow-up webinar two weeks after the main event for debrief and concerns. Push out one-page suggestions. Welcome learners to send situations for feedback.
Measure what issues. Track not just fulfillment ratings, however changes in suggesting, block use, and patient-reported end results after training. Share wins with management to sustain support.
Ethics and equity hurting education
Pain treatment is not simply pharmacology and nerve blocks. It is equity, stigma, and access. Programs that do not touch on prejudice miss out on a core component. People with darker skin typically get much less ample analgesia. Individuals with minimal English efficiency struggle to share discomfort without interpreters. People with a history important usage may obtain disregarded, after that return sicker.
Include quick modules on predisposition, language access, and trauma-informed care. For example, practice making use of a certified interpreter to establish assumptions about tapering or function-focused goals. Normalize screening for state of mind and rest. These behaviors lower differences and improve outcomes.
What to get out of a strong discomfort monitoring certificate course
By the end of a well-constructed pain management certificate course, many medical professionals report a few consistent modifications:
- They default to multimodal strategies and utilize opioids later and for shorter durations. They file risk and reasoning in a manner that takes on scrutiny. They feel comfortable with at the very least one regional technique or non-opioid pathway they did not utilize before. They manage tapering and changes much more with confidence, with fewer adversarial conversations.
Across teams, these modifications appear as shorter ED remains for discomfort presentations, fewer returns for badly managed pain, and extra constant patient education.
Cost, CME, and realistic time commitments
Pricing differs commonly. Numerous hospital-based programs run at marginal expense for staff. External training courses range from a couple of hundred dollars for on-line components to a number of thousand for hybrid programs with hands-on workshops and identified discomfort administration certification. Anticipate 6 to 20 hours of web content for brief training courses, usually spread throughout nights or weekend breaks. If your employer offers CME allowances, a program that provides both hours and an identifiable credential is much easier to justify.
For nurses, some programs meet yearly expertise demands or contribute to scientific ladder factors. For physiotherapists, qualification from a nationwide professional body carries extra value than a generic certificate. For medical professionals, inspect alignment with specialty university CME categories and whether procedural components can be credited.
How to make the learning stick next week
Courses present expertise. Systems and practices equate it right into care. Before you log in or fly out, strategy just how you will use what you learn.
Pick two habits to execute instantly. As an example, take on a conventional ED migraine headache protocol and start offering fascia iliaca blocks on proper hip cracks. Or in facility, start every chronic pain check out with a one-sentence useful goal and record it consistently.
Create a microlibrary. Conserve dosing graphes, permission phrases for nerve blocks, and individual handouts on a common drive or print a little binder. Make it simple for colleagues to take on the same patterns.
Measure your very own modification. For a month, track exactly how typically you prescribe opioids for bone and joint pain, or how many nerve blocks you execute. Share results with your group. Energy expands when you see progress.
Find a companion. Couple with a colleague who likewise finished the pain management training. Debrief as soon as a week for a month. Share misses as well as victories. You will troubleshoot faster together.
A note on chronic discomfort programs and interprofessional partnerships
Short courses hardly ever change chronic discomfort alone. They do, nonetheless, equip you to connect patients to the appropriate resources previously. A physiotherapist that understands pain neuroscience can craft graded exposure strategies that match well with a doctor's medication strategy. A registered nurse who is learnt PCA safety can prevent breathing concession and identify ecstasy early. A GP with discomfort monitoring accreditation can structure tapering plans and describe multidisciplinary discomfort centers when warnings appear.
The most reliable systems straighten expertises. If your area has a relentless discomfort program, ask exactly how your new skills fit their paths. Offer to pilot a joint education evening. Individuals profit when messages match from the waiting room to the ward.
Final thoughts from the facility floor
The worth of pain education appears at little minutes. The young adult with a forearm crack who stays clear of an unneeded opioid manuscript due to the fact that you placed a gentle hematoma block. The older guy with tiles who sleeps via the evening for the first time in a week because you focused on early antiviral treatment and gabapentin with clear application. The middle-aged woman with chronic knee pain who starts a pacing strategy and finds out to gauge progression by staircases climbed, not simply discomfort scored.
Short courses in pain management aid you see those alternatives much faster. Select a program that appreciates your range, evaluates actual abilities, and sustains you after the program ends. Whether you go after a pain management certification for professional acknowledgment or simply to enhance Tuesday's facility, the ideal training makes care much safer, kinder, and extra effective for the people who trust you with their pain.